Online Graduate Nursing Programs
Nurse Administrator
Nurse Educator
Family/Individual Across the Lifespan Nurse Practitioner
Adult Gerontology Acute Care Nurse Practitioner
For information, contact
Dr. Wendy J. Robb, wjrobb@cedarcrest.edu
610-606-4606
Mission of the Graduate Nursing Program
The mission of the Cedar Crest College graduate nursing program is to educate and prepare nurse leaders who will advance evidence-based practice, education, and healthcare delivery to improve health outcomes for individuals, families, and communities within a global context.
Master of Science in Nursing Program
The Master of Science in Nursing (MSN) program is designed to prepare students to function as nurse leaders in a wide variety of practice and educational settings. The program is innovative in approach and design, offering students a part-time, year-round track in Family/Individual Across the Lifespan Nurse Practitioner (FNP) and Adult Gerontology Acute Care Nurse Practitioner (AGACNP) and part- and full-time tracks in Nurse Administrator and Nurse Educator tracks. In the nurse practitioner tracks, the curriculum encourages students to further their clinical expertise, while developing proficiency in the specialties of FNP & AGACNP. Graduates will be prepared to assume leadership positions in a variety of clinical practice roles and will be equipped to influence change within the healthcare delivery systems of the twenty-first century. The nurse administrator and nurse educator tracks foster development of nursing leadership skills that will enable graduates to assess and evaluate nursing and healthcare practice systems, educational methods, and research findings, while also equipping students to develop evidence-based practice changes in healthcare agencies or academic institutions. Graduates will be prepared to continue their education in doctoral programs of study.
The MSN and Bachelor of Science in Nursing to Doctor of Nursing Practice (BSN-DNP) FNP and AGACNP programs are approved by the Pennsylvania State Board of Nursing.
ACEN
The master’s/post-master’s certificate nursing program at Cedar Crest College located in Allentown, PA is accredited by the: Accreditation Commission for Education in Nursing (ACEN) 3390 Peachtree Road NE, Suite 1400, Atlanta, Georgia 30326, (404)975-5000. The most recent accreditation decision made by the ACEN Board of Commissioners for the master’s/post-master’s certificate nursing program is continuing accreditation. View the public information disclosed by the ACEN regarding this program on the ACEN website (www.acenursing.org).
The most recent accreditation decision made by the ACEN Board of Commissioners for the Master of Science in Nursing and Post Master’s Certificate nursing programs is Continuing Accreditation.
View the public information disclosed by the ACEN regarding this program on the ACEN website.
CCNE
The master’s degree program in nursing, Doctor of Nursing Practice program, and post-graduate APRN certificate program at Cedar Crest College are accredited by the Commission on Collegiate Nursing Education, 655 K Street NW, Suite 750, Washington, DC 2001, 202-887-6791. (www.ccneaccreditation.org).
The Cedar Crest College School of Nursing’s facilities are housed in the Hamilton Boulevard Building, a state-of-the-art facility that is one of the finest of its kind in the region. The 34,000 square foot building includes: three multi-media labs including a health assessment lab, a maternal and pediatric lab, and an adult health lab; a fully equipped nursing unit that simulates a hospital environment; a simulation center with 2 adjacent computerized learning mannequin laboratories and a separate control/observation room; a community health lab set up to replicate a home-care environment; convertible classrooms, and conference facilities to accommodate 300 persons. There is a dedicated 3,900 square foot lab area for the graduate nursing programs that includes: a simulation space featuring two high-fidelity simulation rooms, debriefing room, simulated operating room, peri-operative area, 10-bay advanced health assessment lab, student study areas and lockers for student belongings. The Hamilton Boulevard Building provides high speed wireless internet and also houses a computer lab for student use. All nursing faculty offices are located in the Hamilton Boulevard Building.
MSN Admission Requirements
Students are admitted to graduate programs at Cedar Crest College on the basis of individual qualifications. Requests for application materials and all correspondence relating to admission should be addressed to:
Cedar Crest College
School for Adult and Graduate Education
100 College Drive
Allentown, PA 18104-6196
Phone: 610-740-3770
Email: sage@cedarcrest.edu
Fax: 610-740-3786
Online Application Materials: www.cedarcrest.edu/apply
A rolling admissions policy is in effect for this program. Applications are accepted and reviewed on a continuing basis throughout the year.
The general admission requirements for the Master of Science in Nursing Program are as follows:
- Completed online application form
- Bachelor’s degree in nursing from an accredited program
- Minimum of 3.0 grade point average (on a 4.0 scale) in a BSN program
- Active, unencumbered Registered Nurse licensure in Pennsylvania
- Official transcripts from all previously attended institutions of higher education
- Current resume
- Professional goal statement
- Completion of undergraduate statistics, research, and health assessment courses with a grade of C or better
- No clinical experience required. One year preferred.
- Two (2) professional recommendations preferably from nurses with graduate degrees, including: current employer, nursing Professor, or other nursing professional.
- Completion of an interview with the Director of the program and/or representatives from the Graduate Nursing Program Committee.
- Satisfactory scores on the Test of English as a Foreign Language (TOEFL) for all applicants who are non-native English speakers.
- If previous course work was completed outside of the United States, students should have their academic degree validated as equivalent to a degree in the Unites States through a non-profit agency, such as World Education Services www.wes.org
Master of Science in Nursing Program Goals and Expected Learning Outcomes
MSN Program Goals
- Integrate knowledge of theory and research to develop a comprehensive and ethical approach for nursing practice, education, and administration in a global society.
- Utilize advanced clinical knowledge and skill to promote, maintain, and/or restore optimum wellness to clients.
- Articulate the issues and trends that affect the social, economic, political, and institutional forces that influence nursing and health care delivery.
- Critically appraise and utilize scientific, expert, and other sources of knowledge to ensure quality outcomes in the context of evidence-based practice.
- Develop collaborative and inter-professional relationships to improve health outcomes in a variety of settings.
Expected Learning Outcomes by Track
Family/Individual Across the Lifespan Nurse Practitioner
Upon completion of the FNP track the graduate will be able to:
- Provide full scope of evidence-based primary care, utilizing both independent and collaborative approaches, to individuals and families across the lifespan.
- Manage acute and chronic health problems, health promotion activities, disease prevention, and transitional support and end of life care.
- Participate in evidence-based quality improvement initiatives to improve healthcare outcomes.
- Coordinate health care teams and engage in inter-professional collaboration with members of the health care team.
- Advocate for health care systems and policies that reduce health disparities, facilitate access to care and address cultural diversity.
Adult Gerontology Acute Care Nurse Practitioner
Upon completion of the AGACNP track the graduate will be able to:
- Provide full scope of evidence-based care, utilizing both independent and collaborative approaches, to the adult/gerontology population.
- Manage acute, critical, and/or complex chronic health problems, health promotion activities, disease prevention, and transitional support and end of life care.
- Participate in evidence-based quality improvement initiatives to improve healthcare outcomes.
- Coordinate health care teams and engage in inter-professional collaboration with members of the health care team.
- Advocate for health care systems and policies that reduce health disparities, facilitate access to care, and address cultural diversity.
Nurse Educator
Upon completion of the Nurse Educator track the graduate will be able to:
- Create an environment in classroom, laboratory, and clinical settings that facilitate student learning and achievement of desired cognitive, affective, and psychomotor outcomes.
- Recognize the responsibility for helping students develop as nurses and integrate the values and behaviors expected of those who fulfill that role.
- Use a variety of strategies to assess and evaluate student learning in classroom, laboratory and clinical settings, as well as in all domains of learning.
- Formulate program outcomes and design curricula that reflect contemporary health care trends and prepare graduates to function effectively in the health care environment.
- Function as change agents and leaders to create a preferred future for nursing education and nursing practice.
- Maintain competence in the educator role through the commitment to and pursuit of continuous quality improvement.
- Engage effectively in scholarship as an integral component of the nurse educator role.
- Demonstrate knowledge about the educational environment within which the student practices and recognize how political, institutional, social, and economic forces impact the role of nurse educators.
Note: Adapted from the National League for Nursing Core Competencies of Nurse Educators with Task Statements (2012).
Nurse Administrator
Upon completion of the Nurse Administrator track the graduate will be able to:
- Function effectively as a leader within a health care system.
- Use systems thinking to evaluate the impact of nursing decisions on the health care organization as a whole.
- Apply knowledge of health care policy, regulations, economics, budgeting, and finance to improve organizational effectiveness.
- Lead and manage a diverse human workforce.
- Develop collaborative relationships within the health care system, the community and academia.
- Critically appraise best evidence to improve organizational effectiveness and patient outcomes.
- Determine patient care quality improvement goals in accordance with national quality initiatives.
- Use information systems to access and analyze data for use in planning for patient care and health care system processes.
- Apply legal and ethical standards to health care operations.
- Facilitate change within health care organizations.
Program of Study for the Master of Science in Nursing Degree
The progression of the Master of Science in Nursing curriculum encourages students to further their clinical expertise while developing proficiency in the specialties of FNP, AGACNP, Nurse Administrator & Nurse Educator. Nurse Administrator & Nurse Educator graduates will be eligible for certification. Advanced Practice Registered Nurse (APRN) graduates will be eligible for national certification.
The number of credits for the MSN tracks are as follows:
- Adult Gerontology Acute Care Nurse Practitioner (AGACNP) 46 credits
- Family/Individual Across the Lifespan Nurse Practitioner (FNP) 49 credits
- Nurse Educator 37 credits
- Nurse Administrator 37 credits
Graduate Nursing Core Courses
MSN 510 Conceptual and Theoretical Foundations for Nursing (3 credits, 7-week format)
MSN 512 Research for Evidence-Based Nursing Practice (3 credits, 7-week format)
MSN 514 Informatics and Technology in Nursing (3 credits, 7-week format)
MSN 516 Issues and Trends Relevant to Nursing (3 credits, 7-week format)
MSN 520 Vulnerable Populations: Nursing Perspectives (3 credits, 7-week format)
Graduate Nursing Direct Care Courses
MSN 550 Physiology and Pathophysiology for Advanced Practice Nursing Across the Lifespan (3 credits, 14-week format)
MSN 551 Advanced Health & Physical Assessment Across the Lifespan (3 credits = 2 didactic, 1 online lab [56 hours], 14-week format)
MSN 552 Pharmacological Principles of Clinical Therapeutics Across the Lifespan (3 credits, 14-week format)
Specialty Courses
Family/Individual Across the Lifespan Nurse Practitioner
MSN 600 Primary Care of the Family & Individual Across the Lifespan I – Women & Families (3 credits, 14-week format)
MSN 601 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan I – Women & Families (2 credits, 112 clock hours, 14-week format)
MSN 602 Primary Care of the Family & Individual Across the Lifespan II – Infants, Children & Adolescents (3 credits, 14-week format)
MSN 603 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan II – Infants, Children & Adolescents (2 credits, 112 clock hours, 14-week format)
MSN 604 Primary Care of the Family & Individual Across the Lifespan III – Adults & Older Adults (3 credits, 14-week format)
MSN 605 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan III – Adults & Older Adults (4 credits, 224 clock hours, 14-week format)
MSN 606 Primary Care of the Family & Individual Across the Lifespan IV – Adults & Older Adults (3 credits, 14-week format)
MSN 607 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan IV – Adults & Older Adults (5 credits, 280 clock hours, 14-week format)
Adult-Gerontology Acute Care Nurse Practitioner
- MSN 620 Advanced Health Assessment & Clinical Reasoning for the Adult-Gerontology Acute Care Nurse Practitioner (2 credits, 14-week format)
- MSN 621 Clinical Practicum Advanced Health Assessment & Clinical Reasoning for the Adult-Gerontology Acute Care Nurse Practitioner (1 credit, 56 clock hours, 14-week format
- MSN 610 Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses I (3 credits, 14-week format)
- MSN 611 Clinical Practicum Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses I (3 credits, 168 clock hours, 14-week format)
- MSN 612 Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses-II (3 credits, 14-week format)
- MSN 613 Clinical Practicum Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses-II (4 credits, 224 clock hours, 14-week format)
- MSN 614 Adult-Gerontology, Traumatic Injury & Emergency Illnesses Diagnosis & Management (1 credit, 14-week format)
- MSN 615 Clinical Residency (5 credits, 280 clock hours, 14-week format)
Nurse Educator
MSN 531 Curricula in Nursing Education (3 credits, 14-week format)
MSN 532 Nurse Educator Practicum I (4 credits=3 credits didactic and 1 credit clinical [56 clock hours], 14-week format)
MSN 535 Nurse Educator Practicum II (6 credits=3 credits didactic and 3 credits clinical [168 clock hours], 14-week format)
Nurse Administrator
MSN 541 Nursing Care Delivery Systems (3 credits, 14-week format)
MSN 543 Resources for the Delivery of Nursing (4 credits=3 credits didactic and 1 credit clinical [56 clock hours], 14-week format)
MSN 545 Nurse Administrator Practicum (6 credits=3 credits didactic and 3 credits clinical [168 clock hours], 14-week format)
Post Master’s Online Certificate Program
Cedar Crest College offers Post Master’s Online Certificates in the following specialties:
Nursing Administrator 13 credits
Nursing Educator 13 credits
Adult-Gerontology Acute Care Nurse Practitioner (AGACNP) 22 credits
Family/Individual Across the Lifespan Nurse Practitioner 25 credits
The Post-Master’s Advanced Practice Registered Nurse (APRN) Certificate Program is for registered nurses who hold a Master of Science Degree in Nursing and are interested in specializing in another area of study. Graduates of the Post-Master’s APRN Certificate Program are expected to meet the master’s program goals, and the expected learning outcomes of the specialty NP tracks. Graduates of the Post-Master’s Certificate Program are eligible for national certification.
The Post-Master’s non-APRN Certificate Program (nurse administrator and nurse educator) is for registered nurses who hold a Master of Science Degree in Nursing and are interested in specializing in another area of study. Graduates of the non-APRN Certificate Program are expected to meet the master’s program goals, and the expected learning outcomes of the nurse administrator and nurse educator tracks. Graduates of the Post-Master’s Certificate Program are eligible for certification.
Post Master’s Certificate Admission Requirements
The admission criteria for Post Master’s Certificates are as follows:
- Completed online application form
- Master’s degree in Nursing from an accredited program
- Minimum 3.0 grade point average (on a 4.0 scale) in a MSN program
- Active, unencumbered Registered Nurse licensure in Pennsylvania
- Official transcripts from all previously attended institutions of higher education
- Current resume
- Professional goal statement
- No clinical experience required. One year preferred.
- Two (2) professional recommendations preferably from nurses with graduate degrees, including: current employer, nursing Professor, or other nursing professional.
- Completion of an interview with the Director of the program
- Satisfactory scores on the Test of English as a Foreign Language (TOEFL) for all applicants who are non-native English speakers
- If previous course work was completed outside of the United States, students should have their academic degree validated as equivalent to a degree in the Unites States through a non-profit agency, such as World Education Services www.wes.org
Post Master’s Certificate Program of Study
All entering Post-Master’s APRN Certificate students must show evidence of having completed three (3) separate, comprehensive graduate-level courses in advanced pathophysiology, advanced health assessment, and advanced pharmacology. Post-Master’s APRN Certificate students who have not satisfactorily completed such courses will be required to complete MSN 550, MSN 551, and MSN 552 as non- matriculated students prior to admission to the Post- Master’s Certificate program. All students entering the Post-Master’s APRN Certificate program will have a gap analysis performed to determine their individual plans of study.
Nurse Educator Specialty Courses
MSN 531 Curricula in Nursing Education (3 credits)
MSN 532 Nurse Educator Practicum I (4 credits=3 credits didactic and 1 credit clinical [56 clock hours], 14-week format)
MSN 535 Nurse Educator Practicum II (6 credits: 3 credits didactic, 3 credits clinical [168 clock hours])
Nurse Administrator Specialty Courses
MSN 541 Nursing Care Delivery Systems (3 credits)
MSN 543 Resources for the Delivery of Nursing (4 credits=3 credits didactic, 1 credit clinical [56 clock hours])
MSN 545 Nurse Administrator Practicum (6 credits=3 credits didactic, 3 credits clinical [168 clock hours])
Family/Individual Across the Lifespan Nurse Practitioner Specialty Courses
MSN 600 Primary Care of the Family & Individual Across the Lifespan I – Women & Families (3 credits)
MSN 601 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan I – Women & Families (2 credits) – 112 clock hours
MSN602 Primary Care of the Family & Individual Across the Lifespan II – Infants, Children & Adolescents (3 credits)
MSN 603 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan II – Infants, Children & Adolescents (2 credits) – 112 clock hours
MSN 604 Primary Care of the Family & Individual Across the Lifespan III – Adults & Older Adults (3 credits)
MSN 605 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan III – Adults & Older Adults (4 credits) – 224 clock hours
MSN 606 Primary Care of the Family & Individual Across the Lifespan IV – Adults & Older Adults (3 credits)
MSN 607 Clinical Practicum Primary Care of the Family & Individual Across the Lifespan IV – Adults & Older Adults (5 credits) – 280 clock hours
Adult-Gerontology Acute Care Nurse Practitioner Specialty Courses
MSN 620 Advanced Health Assessment & Clinical Reasoning for the Adult-Gerontology Acute Care Nurse Practitioner (2 credits, 14-week format)
MSN 621 Clinical Practicum Advanced Health Assessment & Clinical Reasoning for the Adult-Gerontology Acute Care Nurse Practitioner (1 credit, 56 clock hours, 14-week format
MSN 610 Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses I (3 credits)
MSN 611 Clinical Practicum Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses I (3 credits) – 168 clock hours
MSN612 Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses-II (3 credits)
MSN 613 Clinical Practicum Adult-Gerontology Diagnosis & Management of Chronic & Acute Illnesses-II (4 credits) – 224 clock hours
MSN 614 Adult-Gerontology, Traumatic Injury & Emergency Illnesses Diagnosis & Management (1 credit)
MSN 615 Clinical Residency (5 credits) – 280 clock hours (20 hours/week)
On Campus Immersion Experiences
Nurse Educator and Nurse Administrator Tracks
The Nurse Educator, Nurse Administrator and Nurse Practitioner tracks at Cedar Crest College include an optional On Campus Immersion Experience which provides students with the opportunity to become familiar with campus resources, meet faculty, and network with peers. Since students are admitted on a rolling basis, they will be enrolled in the Graduate Nursing Orientation and Resource course during the semester in which they begin classes.
The initial On Campus Immersion will be held at Cedar Crest College in August.
Nurse Practitioner Tracks
The Nurse Practitioner tracks at Cedar Crest College include On Campus Immersion Experiences which provide students with the opportunity to meet faculty, network with peers, practice clinical skills in our state-of-the-art simulation settings and learn and grow as advanced practitioners.
The On Campus Immersion II will be held in October-Year Two. This will be a two-day experience and is required before any student may attend clinical practicum experiences
Provisional Acceptance
Provisional acceptance will be considered for students who do not meet all admission criteria. Once granted provisional acceptance into the program, the student must maintain a 3.0 GPA in the first 6 credits. Provisional acceptance is intended to allow students the opportunity to verify their level of readiness for graduate study.
Visiting Student
Candidates may apply as a non-degree visiting student and take a maximum of 6 credits from the Graduate Nursing Core or Direct Care courses. Upon completion of those credits, the student must apply for admission.
Matriculation
Matriculation is required for any student who plans to receive financial aid and/or a graduate degree. A student applies for matriculation by submitting a completed application for admission to the School of Adult and Graduate Education. After submitting a complete application, students receive a letter from the College informing them of the decision concerning their acceptance as a degree candidate. Students are matriculated into the program once they have registered for classes during their first semester of academic study. The date of matriculation is the first day of classes in the term in which the student is enrolled after having satisfied all matriculation requirements.
Graduate programs may permit non-matriculated and visiting students to enroll in graduate courses on a case-by-case basis. In the event that a graduate course reaches its enrollment maximum, matriculated students are given preference over non-matriculated students.
Transfer Credit Policy
Students entering the program may transfer up to 9 credits of coursework at the discretion of the Program Director. Of these 9 credits, a maximum of 6 credits may be from the “3 P’s” courses- Advanced Pharmacology, Advanced Physical Assessment and Advanced Pathophysiology. The transferred coursework, however, must be equivalent to courses listed in the curriculum and must have been completed within five years of the date of enrollment in the program (the first day of classes of a student’s first academic year). In order for course work to be considered for transfer, students must submit a course description, course syllabus if available, and transcript indicating the student’s achieved grade for the course. Once matriculated in the program, students will not receive any credit for coursework taken at another institution.
Transfer credits are not accepted for the Post-Master’s certificate programs in Nursing Administration & Nursing Education.
Please see Policies and Information below that apply to the MSN & DNP Programs (Maximum Period of Candidacy, Leave of Absences, Completion of Graduate Program, Expenses, Advising, Sigma Theta Tau – The International Nursing Honor Society Theta Rho Chapter
Doctor of Nursing Practice Program
The Doctor of Nursing Practice (DNP) Program prepares expert nurse clinicians and executive leaders for the highest level of practice to improve health outcomes for individuals and populations. Graduates will be employed in primary care settings, hospitals, and other acute care settings, public health agencies, and schools of nursing.
Cedar Crest College currently offers two nurse practitioner tracks for the BSN-DNP program: Family/Individual Across the Lifespan Nurse Practitioner (FNP) and Adult-Gerontology Acute Care Nurse Practitioner (AGACNP); and the Nurse Anesthesia Track (NAP) Please see NAP-specific program information in next section
The number of credits for the BSN-DNP program varies depending on track. After completing the coursework for the Master of Science in Nursing degree, students can smoothly transition into the doctoral portion of the BSN-DNP program.
The DNP program has a curricular emphasis on evidence-based practice which prepares graduate students to translate and integrate current best practices, contribute to nursing’s unique body of knowledge, and advance the profession of nursing. All DNP students must complete and successfully present a scholarly practice project and complete a minimum of 1,000 hours of post-baccalaureate clinical/practicum hours. In addition to a minimum of 728 clinical hours required for the successful completion of the nurse practitioner specialty track, there is a minimum of 336 documented practicum hours required which are dedicated to the planning, proposal, implementation, evaluation, and dissemination of an evidence- based scholarly project demonstrating the attainment of the Advanced-level essentials. Students must meet course requirements, DNP Project requirements, and all clinical/practicum hour requirements in order to successfully complete the program.
Doctor of Nursing Practice Program Goals and Expected Learning Outcomes
Doctor of Nursing Practice (DNP) Program Goals
The DNP curriculum for BSN prepared students is designed with courses sequentially organized to promote student achievement of program goals. Expected learning outcomes and course objectives in each course guide the selection of learning activities and evaluation methods throughout the curriculum. Each course builds on the knowledge, skills, and abilities students developed in previous course work. Over the plan of study in the DNP program, students are expected to attain the following five overarching goals:
- Evaluate health outcomes of individuals, communities, and populations in complex healthcare systems through evidence-based practice.
- Integrate theoretical and scientific knowledge to provide high quality health care that is ethical, safe, and evidence-based to diverse individuals, communities, and populations.
- Translate evidence to guide practice and improve health outcomes and systems of care.
- Influence healthcare policy relative to social, ethical, legal, economic, and political issues that impact nursing.
- Direct high quality, cost-effective care in collaborative relationships with other health care providers.
DNP Expected Learning Outcomes
Graduates of the DNP program will be able to:
- Develop cost-effective innovations to improve health through the synthesis of theoretical, philosophical, ethical, and empirical knowledge.
- Utilize leadership skills within complex health systems to improve safe, cost-effective, and quality healthcare for diverse populations.
- Act as a practice scholar to design, implement, and translate evidence to promote safe, timely, effective, efficient, equitable, and patient-centered care.
- Engage in evidence-based advanced-nursing practice and evaluate innovative approaches to care delivery for individuals, communities and populations.
- Utilize and evaluate health information systems for improvement and transformation of clinical, research, and administrative practices.
- Employ strategic leadership skills to analyze, develop, and implement health care policy on local, regional, national, and global levels.
- Partner with others to develop interactive interprofessional collaborative teams to improve health outcomes among diverse populations.
Program of Study for the Doctor of Nursing Practice Online Degree
DNP Courses
DNP 801 Methods for Scholarly Inquiry (3 credits)
DNP 802 Biostatistics for Evidence-based Practice (3 credits)
DNP 803 Theories of Leadership & Organization (3 credits)
DNP 804 Health Policy, Economics, & Finance (3 credits)
DNP 805 Foundation for Transformation: Translating Evidence into Practice (3 credits)
DNP 806 Evaluation Methods for Safety & Quality Improvement (3 credits)
DNP 850 DNP Project I (4 credits) 1 didactic credit, 3 practicum credits
DNP 851 DNP Project II (4 credits) 1 didactic credit, 3 practicum credits
DNP 852 DNP Project III (2 credits)
DNP 853 DNP Project IV Maintenance of Candidacy if needed (1 credit)
Policies and Information for MSN & BSN-DNP Programs*
*Please see the School of Nursing Graduate Handbook and Graduate Nursing Clinical and Preceptor Guidelines for additional policies and information
Maximum Period of Candidacy
It is expected that all students will complete program requirements within seven academic years unless otherwise approved by the Director of the program.
Leaves of Absence
Students wishing to take a leave of absence from the program may request to do so in writing to the Director of the program. The granting of the requested leave is at the discretion of the Director and the Graduate Nursing Program Committee. A granted leave of absence has no bearing on the maximum period of candidacy.
Completion of the Graduate Program and Graduation
To successfully complete the Master of Science in Nursing Program, a student must adhere to the following:
- Successfully complete all the requirements for the program.
- Maintain a minimum cumulative GPA of 3.0.
- Apply to the Registrar for graduation by the published application deadline.
- Complete an electronic end of program survey or participate in an exit interview.
- Fulfill all financial responsibilities to the College.
Graduate 2024-2025 Tuition and Fees
Nursing Graduate Tuition, per credit $670.00
Doctor of Nursing Practice (DNP), per credit $795
Activity Fee, per semester $20.00
Full-Time Technology Fee, per semester $125.00
Part-Time Technology Fee, per semester $75.00
MSN Clinical Fees per course (MSN 532, 535, 543, 545, 551, 601, 603, 605, 607, 611, 613, 615, 621) $300
OCI #2 Fee $150
Family Nurse Practitioner Rosh Review/ Board Prep Fees: $600 Family Nurse Practitioner iHuman and Meta Women’s Health $695
Adult/Gero Nurse Practitioner Rosh Review/ Board Prep Fees $750
Adult/Gero Nurse Practitioner iHuman $165
Note: The College reserves the right to change fees and charges as necessary. Books, supplies, lab materials and other program costs are not included in the tuition.
Expenses
Graduate nursing students are responsible for all fees involved when obtaining the clinical requirements, secured electronic file management, clinical attire, equipment, books, and professional and scholarly activities. Note: The College reserves the right to change fees and charges, as necessary.
Advising
A student accepted to the Graduate Nursing Program will be assigned an academic advisor who will work with the student in planning the program of study, and as a mentor for professional development. Faculty advisors are assigned by the Director of the program. Students wishing to request a specific faculty advisor should submit this request in writing to the Director.
Graduate Nursing Resources
Upon acceptance into the program and registration for courses, new students are sent an invitation to join the Graduate Resources modules via Canvas that is specifically reserved for students in the graduate nursing program. This resource contains important information including program handbooks, hyperlinks to a variety of college resources, and more.
Graduate Student Handbook
Each student has access to the Graduate Nursing Student Handbook in the Graduate Resource Modules. The purpose of the handbook is to provide students with information pertaining to the curricular requirements and policies and procedures associated with the program. Students are responsible for understanding the information in the School of Nursing Graduate Handbook. Questions regarding the content of the handbook should be directed to either the student’s faculty advisor or the Director of the program.
Sigma Theta Tau, The International Nursing Honor Society Theta Rho Chapter
The Cedar Crest College Nursing Honor Society was established in the Spring of 1981. The first group was inducted into the Society on April 23, 1981. Through the efforts of many Society members, by-laws were developed according to the recommendations of Sigma Theta Tau, the International Honor Society for Nursing. In April 1986, the Nursing Honor Society was chartered as Theta Rho Chapter of Sigma Theta Tau.
As described in the Chapter by-laws, the purposes of the Nursing Honor Society are to: recognize superior achievement and scholarship, recognize the development of leadership qualities, foster high professional standards, encourage creative work, and strengthen commitment to the ideals and purposes of the profession.
To apply for membership in the Theta Rho Chapter, the graduate student must meet the following criteria:
- Have completed at least ¼ of the program of study
- Have a minimum GPA of 3.5
- Meet the expectation of academic integrity.
Graduate students who meet eligibility criteria may apply for membership online at www.nursingsocitey.org. Theta Rho will review the application and notify the candidate of their acceptance. The Induction Ceremony is held in the Spring semester.
Based on survey data for more online course offerings, the graduate nursing program transitioned to an online format in spring 2016.
BSN-DNP Nurse Anesthesia Program
Bimpe Adenusi, Ph.D., APRN, CRNA, CNE, FAANA.
Program Director
bimpe.adenusi@cedarcrest.edu
Mission of the Graduate Nursing Program
The mission of the Cedar Crest College graduate nursing program is to educate and prepare nurse leaders who will advance evidence-based practice, education, and healthcare delivery to improve health outcomes for individuals, families, and communities within a global context.
The Cedar Crest College Nursing Department’s facilities are housed in the Hamilton Boulevard Building, a state-of-the-art facility that is one of the finest of its kind in the region. The 34,000 square foot building includes: three multi-media labs including a health assessment lab, a maternal and pediatric lab, and an adult health lab; a fully equipped nursing unit that simulates a hospital environment; a simulation center with 2 adjacent computerized learning mannequin laboratories and a separate control/observation room; a community health lab set up to replicate a home-care environment; convertible classrooms, and conference facilities to accommodate 300 persons. There is a dedicated 3,900 square foot lab area for the graduate nursing programs that includes: a simulation space featuring two high-fidelity simulation rooms, debriefing room, simulated operating room, peri-operative area, 10-bay advanced health assessment lab, student study areas and lockers for student belongings. The Hamilton Boulevard Building provides high speed wireless internet and also houses a computer lab for student use. All nursing faculty offices are located in the Hamilton Boulevard Building.
BSN to DNP Nurse Anesthesia Program
The Doctor of Nursing Practice Nurse Anesthesia Program is a 36-month full time program designed for the post baccalaureate RN seeking certification in anesthesia and doctoral education. Nurse anesthesia students will have the opportunity to learn in a hands-on environment to promote more effective skill development. This curriculum integrates didactic coursework with over 2,000 hours of clinical, ensuring that students administer more than 800 anesthetics to patients undergoing a wide variety of surgical and/or diagnostic procedures.
Accreditation Status
The Cedar Crest College Nurse Anesthesia Program is fully accredited by the Council on Accreditation of Nurse Anesthesia Education Program, which is recognized by the US Department of Education and the Council for Higher Education Accreditation (CHEA).
Council on Accreditation of Nurses Anesthesia Educational Programs
10275 W. Higgins Road, Suite 906
Rosemont, IL 60018-5603
(224) 275-9130
accreditation@coacrna.org
http://coacrna.org
The master’s degree program in nursing and Doctor of Nursing Practice program at Cedar Crest College are accredited by the Commission on Collegiate Nursing Education (http://www.ccneaccreditation.org).
BSN to DNP Nurse Anesthesia Program (NAP) Goals:
The BSN to DNP NAP curriculum integrates didactic course work with hands on simulated activity for the students. Course objectives in each course guide the selection of learning activities and evaluation methods throughout the curriculum. Each course builds on the knowledge, skills, and abilities students developed in previous course work. Over the plan of study in the BSN to DNP NAP, students are expected to attain the following eight overarching goals:
- Demonstrate advanced knowledge and competence in nurse anesthesia practice in various health care settings for patients in all acuity levels.
- Critically examine and demonstrate the ability to apply findings from scientific literature as a basis for informed nurse anesthesia practice.
- Formulate and implement physiologically sound anesthesia techniques tailored to patient physical status and age.
- Identify researchable problems in nurse anesthesia practice and conduct systematic evaluation of evidence.
- Contribute to new knowledge generation through participation in anesthesia research.
- Participate in the development of clinical, administrative, and educational roles for advanced practice nurses through didactic and clinical coursework.
- Develop collaborative working relationships with members of our community of interest including surgical and anesthesia teams to enhance patient safety.
- Develop and make available faculty expertise for the benefit of the local, regional national and international communities.
BSN to DNP Nurse Anesthesia Program (NAP) Expected Learning Outcomes
At the completion of the program the graduate will be prepared to:
- Conduct and document a comprehensive and systematic assessment of health and illness parameters in complex situations, incorporating diverse and culturally sensitive approaches.
- Obtain and document informed consent including risks, benefits, and anesthesia alternatives.
- Evaluate the patient’s physical and psychological status identifying abnormalities that will have implications on the anesthesia care plan, including evaluation of all laboratory, radiographic, and other diagnostic test data.
- Develop and execute an appropriate anesthesia care plan based on the patient’s condition and the surgical/diagnostic procedure, including effective utilization of fluids and blood products.
- Perform comprehensive and appropriate equipment checks and position or supervise positioning of patients to assure optimal physiologic function and patient safety.
- Design, implement, and evaluate therapeutic interventions based on scientific knowledge and emerging approaches to nurse anesthesia practice and healthcare delivery to promote optimal outcomes.
- Use and interpret a broad variety of monitoring modalities including electronic monitors, taking appropriate action based on sound principle of anesthesia management.
- Recognize and evaluate physiologic responses to the anesthetic, implementing appropriate action that reflects the use of sound physiologic and pharmacologic principles consistent with practice standards and policies.
- Perform within appropriate medical, legal, and ethical standards of anesthesia practice, accepting responsibility and accountability for own practice, recognizing personal and professional strengths and limitations, and taking appropriate actions consistent with valid self-awareness.
- Develop and sustain therapeutic relationships with patients and interprofessional collaboration to facilitate optimal care and patient outcomes.
- Evaluate the post-anesthetic course of the patient and recommend a course of action directed toward correcting any anesthesia-related complications.
- Demonstrate advanced levels of clinical reasoning and judgment, systems thinking, and accountability in designing, delivering, and evaluating evidence-based care to improve patient outcomes
- Demonstrate active professional commitment and involvement in the state organization for nurse anesthetists, and active commitment and involvement in quality management activities.
- Provide leadership or serve as a resource person to support other nurses to achieve excellence in nursing practice and to assure quality patient care.
- Advocate for anesthesia care and health care practice change through active involvement in fiscal issues, policy development and political processes.
- Utilize information systems and technology to improve patient care and healthcare systems.
- Disseminate research evidence
Doctor of Nursing Practice Program
The Doctor of Nursing Practice (DNP) Program prepares expert nurse clinicians and executive leaders for the highest level of practice to improve health outcomes for individuals and populations. Graduates will be employed in primary care settings, hospitals, and other acute care settings, public health agencies, and schools of nursing.
The DNP program has a curricular emphasis on evidence-based practice which prepares graduate students to translate and integrate current best practices, contribute to nursing’s unique body of knowledge, and advance the profession of nursing. All NAP students must complete and successfully present a scholarly practice project and complete a minimum of 336 documented practicum hours in addition to their anesthesia hours. The DNP practicum hours are dedicated to the planning, proposal, implementation, evaluation, and dissemination of an evidence- based scholarly project demonstrating the attainment of the DNP essentials. Students must meet course requirements, DNP Project requirements, and all clinical/practicum hour requirements in order to successfully complete the program.
Doctor of Nursing Practice (DNP) Program Goals
The DNP curriculum for BSN prepared students is designed with courses sequentially organized to promote student achievement of program goals. Expected learning outcomes and course objectives in each course guide the selection of learning activities and evaluation methods throughout the curriculum. Each course builds on the knowledge, skills, and abilities students developed in previous course work. Over the plan of study in the DNP program, students are expected to attain the following five overarching goals:
- Evaluate health outcomes of individuals, communities, and populations in complex healthcare systems through evidence-based practice.
- Integrate theoretical and scientific knowledge to provide high quality health care that is ethical, safe, and evidence-based to diverse individuals, communities, and populations.
- Translate evidence to guide practice and improve health outcomes and systems of care.
- Influence healthcare policy relative to social, ethical, legal, economic, and political issues that impact nursing.
- Direct high quality, cost-effective care in collaborative relationships with other health care providers.
DNP Expected Learning Outcomes
Graduates of the DNP program will be able to:
- Develop cost-effective innovations to improve health through the synthesis of theoretical, philosophical, ethical, and empirical knowledge.
- Utilize leadership skills within complex health systems to improve safe, cost-effective, and quality healthcare for diverse populations.
- Act as a practice scholar to design, implement, and translate evidence to promote safe, timely, effective, efficient, equitable, and patient-centered care.
- Engage in evidence-based advanced-nursing practice and evaluate innovative approaches to care delivery for individuals, communities, and populations.
- Utilize and evaluate health information systems for improvement and transformation of clinical, research, and administrative practices.
- Employ strategic leadership skills to analyze, develop, and implement health care policy on local, regional, national, and global levels.
- Partner with others to develop interactive interprofessional collaborative teams to improve health outcomes among diverse populations.
Admission Requirements
- Graduation from an accredited nursing program.
- The program requires the student to have a bachelor’s degree in nursing. All BSN courses must be completed prior to the application deadline.
- An unencumbered RN License is required. PA and NJ licensure must be documented prior to starting the program.
- Must have one full year of intensive care experience in the United States prior to application deadline.
- Certification in Critical Care Nursing (CCRN) is mandatory.
- Applicants should have a GPA higher than 3.2 out of 4.0 for all undergraduate or graduate degrees. No GRE is required.
- All applicants must have successfully completed Anatomy and Physiology I & II, Chemistry, and Research with a grade B or better.
Documents Requirements for Application
- Three current letters of recommendation: an academic reference, a supervisor, and a mentor/colleague.
- Official transcripts for ALL schools attended after high school regardless of number of credits.
- Advanced Cardiac Life Support (ACLS) certification, Pediatric Advanced Life Support (PALS), Basic Life Support (BLS) from the American Heart Association, and Certification in Critical Care Nursing (CCRN).
- Essay delineating personal goals of graduate study in less than 500 words.
- Documentation of an observational experience with a Certified Registered Nurse Anesthetist (CRNA)
- Interview with the Admissions Committee.
- Current Curriculum Vitae (CV)
Curriculum
The Doctor of Nursing Practice Nurse Anesthesia Program is a 36-month full time program designed for the post baccalaureate RN seeking certification in anesthesia and doctoral education. Nurse anesthesia students will have the opportunity to learn in a hands-on environment to promote more effective skill development. This curriculum integrates didactic coursework with over 2,000 hours of clinical, ensuring that students administer more than 800 anesthetics to patients undergoing a wide variety of surgical and/or diagnostic procedures.
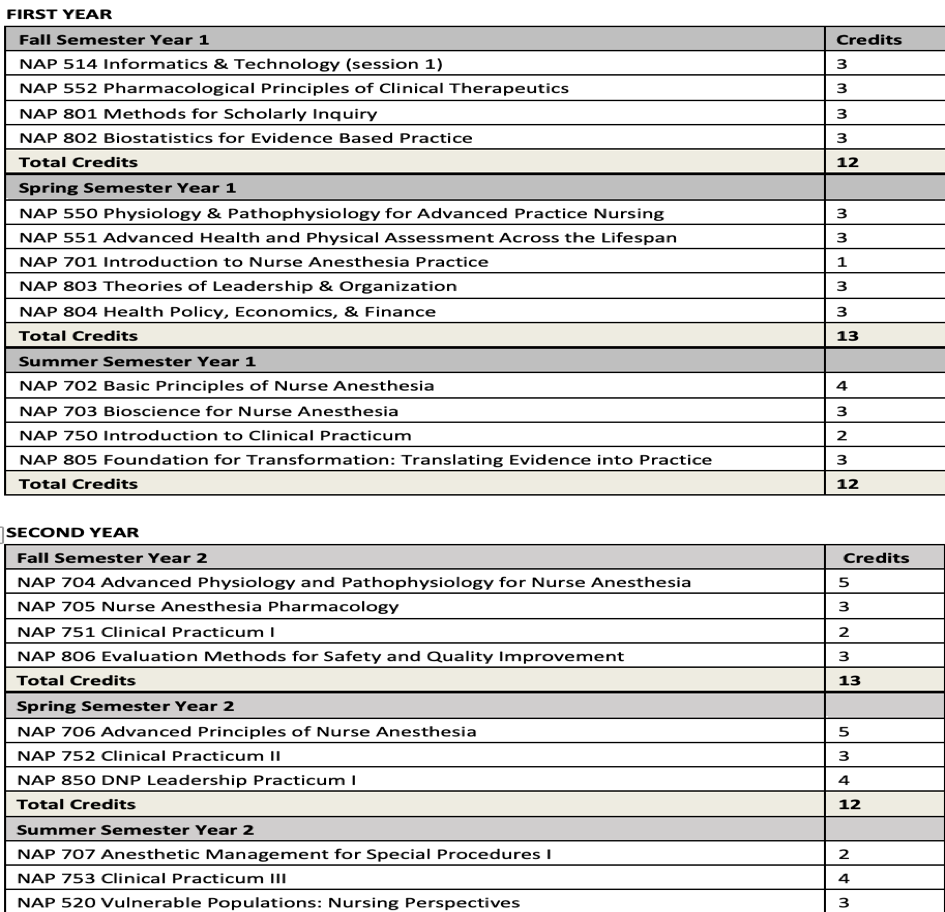
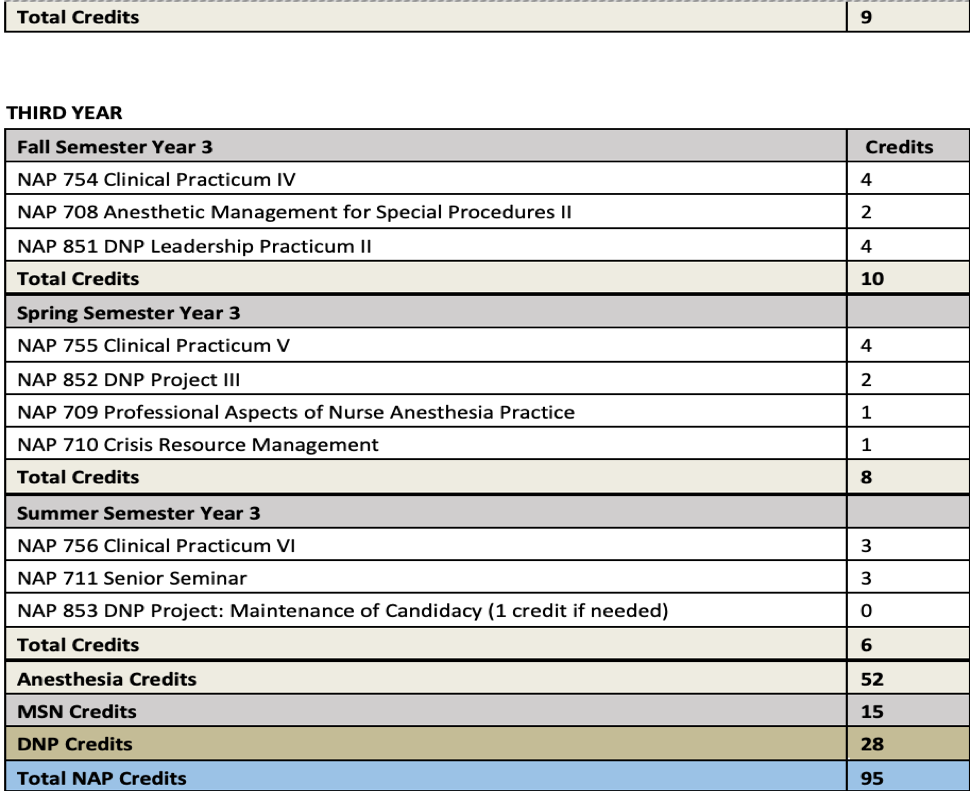
First Year
Students are predominantly in the didactic phases of the curriculum in addition to high fidelity simulation starting in the third semester. Students will develop airway management skills, positioning, patient safety, medication administration and sequence development, among other skills prior to starting clinical practicum.
Second Year
Students have a mix of didactic, simulation and clinical practicum during the second year. The student becomes more familiar with the operating room environment and will apply theory to practice. DNP Leadership Practicum I is in the spring semester which combines practicum experiences with scholarly activities to provide in-depth learning to develop a proposal for the DNP project.
Third Year
In the third year, students continue their clinical practicum and simulation, finalize the DNP project and prepare for the National Certification Exam with on-campus mandatory study days throughout the year.
Employment during the Program
Students are not permitted to be employed during the first two semesters of the Program without prior authorization as set forth in this Handbook. Commencing as of the third semester, Students are not permitted to be employed by any third party through the date of graduation. Under no circumstances may a student be employed as a nurse anesthetist
Graduate Nursing Core Courses Online (15 credits)
NAP 514 Informatics & Technology in Nursing
NAP 520 Vulnerable Populations: Nursing Perspectives
NAP 550 Physiology & Pathophysiology for Advanced Practice Nursing
Across the Lifespan
NAP 551 Advanced Health & Physical Assessment Across the Lifespan
NAP 552 Pharmacological Principles of Clinical Therapeutics Across the Lifespan
DNP Courses (28 credits)
DNP 801 Methods for Scholarly Inquiry (3 credits)
DNP 802 Biostatistics for Evidence-based Practice (3 credits)
DNP 803 Theories of Leadership & Organization (3 credits)
DNP 804 Health Policy, Economics, & Finance (3 credits)
DNP 805 Foundation for Transformation: Translating Evidence into Practice (3 credits)
DNP 806 Evaluation Methods for Safety & Quality Improvement (3 credits)
DNP 850 DNP Project I (4 credits) – 1 didactic credit, 3 clinical credits
DNP 851 DNP Project II (4 credits) – 1 didactic credit, 3 clinical credits
DNP 852 DNP Project III (2 credits)
DNP 853 DNP Project IV – Maintenance of Candidacy (1 credit)
Nurse Anesthesia Core Courses on campus (52 credits)
NAP 701 Introduction to Nurse Anesthesia Practice
NAP 702 Basic Principles of Nurse Anesthesia
NAP 703 Bioscience for Nurse Anesthesia
NAP 704 Advanced Physiology & Pathophysiology for Nurse Anesthesia
NAP 705 Nurse Anesthesia Pharmacology
NAP 706 Advanced Principles of Nurse Anesthesia
NAP 707 Anesthetic Management for Special Procedures I
NAP 708 Anesthetic Management for Special Procedures II
NAP 709 Professional Aspects of Nurse Anesthesia Practice
NAP 710 Crisis Resource Management
NAP 711 Senior Seminar
NAP 750 Introduction to Clinical Practicum
NAP 751 Clinical Practicum I
NAP 752 Clinical Practicum II
NAP 753 Clinical Practicum III
NAP 754 Clinical Practicum IV
NAP 755 Clinical Practicum V
NAP 756 Clinical Practicum VI
Transfer Credits
See Graduate Program Transfer Credit Policy
Financial Considerations
Graduate 2024-2025 Tuition and Fees
NAP Application Fee $50.00
NAP Admission Deposit $1,500.00
NAP Tuition, per credit $1,268.00
Student Activity Fee, per semester $20.00
Full-Time Technology Fee, per semester $125.00
Part-Time Technology Fee, per semester $75.00
Library Resource Fee, per semester $334
Clinical Fee, per semester $334
NAP Bundle Fee, per semester $1,000
Personal Point of Care Ultrasound ~ $2500
NAP-DNP course fee, per semester $1,000 (NAP 850, 851, 852)
NAP Graduation Fee $1,000
Note: The College reserves the right to change fees and charges as necessary. Books, supplies, and other program costs are not included in the tuition. The deposit is credited toward the tuition cost for the first semester.
Please refer to the College’s website. BSN to DNP Nurse Anesthesia Program
Financial Aid
Please refer to the College’s website. BSN to DNP Nurse Anesthesia Program
Liability Insurance
All students must obtain AANA Liability Insurance. Please refer to the following website:
AANA Liability Insurance
Housing
On-campus housing is offered at CCC for female and male undergraduates and graduates students admitted through the School of Adult and Graduate Education based on availability. Please contact for more information:
Office of Residence Life
100 College Drive
Allentown, PA 18104
610-606-4603
Fax: 610-740-3789
reslife@cedarcrest.edu
Miscellaneous Expenses
Please refer to the NAP website for miscellaneous expenses. Miscellaneous Expenses
All students are expected to have a personal electronic device to take notes and in class examinations. Visit Personal Electronic Device for computer discounts. See computer specifications:
All students are required to become associate members of the American Association of Nurse Anesthetists and maintain membership throughout their educational program. Associate membership in the AANA entitles a student to receive the AANA Journal, the AANA Bulletin Professional Activities, and to attend national meetings at discounted costs. Applications for membership in the AANA are processed during the spring semester of the first year.
Clinical Requirements
Students are required to provide the following documentation in order to participate in clinical experiences:
- Completed health forms
- Drug and Alcohol Tests
- Child Abuse History Clearance
- FBI Criminal History Clearance
- PA Criminal History Clearance
- Valid BLS, ACLS and PALS Certification (only accepted through the AHA)
- Proof of Health Insurance
- Current Nursing License in PA, DE and NJ
- Immunizations, Titers, Current PPD, and Influenza Vaccine
These documents and requirements are due prior to admission to the Nurse Anesthesia Program. Documents are uploaded to www.castlebranch.com. Students will receive detailed instructions on this process from the Clinical Liaison once admitted into the program. Castlebranch will notify students if anything is expired or needs to be updated. Students not in compliance will not be allowed to attend class and will be dropped from the course. Late clearances cannot be accepted.
Substance Use Policy
- The substance abuse policy is consistent with the College’s policies on alcohol and drugs as stated in the Cedar Crest College Student Handbook. A student is subject to disciplinary action, including potential dismissal from the College and/or the nursing program if the student violates guidelines stipulated in these policies.
- The intent of the School of Nursing’s Substance Use Policy is to provide a mechanism for nursing students with chemical dependency to receive appropriate counseling, treatment and monitoring without necessitating a withdrawal from the nursing program.
- All students must submit a drug and alcohol test as part of the health requirements for entry into, and continuation, in the program (See Health Requirements section of this handbook). Students who test positive at any point in time will be referred to the Pennsylvania Nurse Peer Assistance Program (PNAP) www.pnap.org.
- The School of Nursing will conduct random drug testing of students each semester. If selected, a student must report to the designated testing facility within 24 hours for a drug and alcohol test. The School of Nursing will assume the cost of random testing. Refusal to report for testing within the 24-hour time frame may result in dismissal from the nursing program. Students who test positive at any point in time will be referred to the Pennsylvania Nurse Peer Assistance Program (PNAP) www.pnap.org.
- Students who test positive may be denied admission or dismissed from the nursing program.
- In the event that a student admits to a chemical dependency or exhibits behavior consistent with consumption of mood-altering chemicals that threaten the safety of others, nursing faculty reserve the right to request the immediate removal from the classroom, clinical/laboratory area.
a. The Dean of the School of Nursing will be notified as soon as possible.
b. The student will be sent for immediate body fluid testing. If the student fails to comply, the student will be subject to dismissal according to School of Nursing policy. - If the student tests positive for substance use or admits to chemical dependency, the Dean of the School of Nursing will notify the Pennsylvania Nurse Peer Assistance Program (PNAP) www.pnap.org. The Pennsylvania Nurse Peer Assistance Program will make a recommendation based on their findings and share these recommendations with the Dean.
a. The student must comply with the Pennsylvania Nurse Peer Assistance Program’s recommendations. Failure to comply with these recommendations will result in dismissal from the nursing program.
b. Compliance with PNAP’s recommendations does not guarantee continuation in the nursing program. The student may not participate in any nursing clinical/laboratory course(s) until PNAP’s recommendations are reviewed by the Dean of the School of Nursing and/or Provost.
c. It may be necessary for the student to take a leave of absence from the nursing program.
d. The student shall assume responsibility for informing their current employer of all information relevant to this matter.
e. The student shall assume responsibility for all expenses related to evaluation and/or treatment as recommended by the Pennsylvania Nurse Peer Assistance Program. - Students must comply with all policies and procedures of affiliate sites, which include, but are not limited to the passing of any drug and alcohol screening procedures.
Progression Policy
Any student receiving less than a final grade of B in any didactic course in the NAP curriculum has not achieved acceptable academic performance. Didactic courses in which students have earned less than a B may not be repeated, and failure of an NAP Course will result in dismissal from the NAP Program. Because of the design of the NAP curriculum, didactic anesthesia courses are only offered once a year and due to the design of the NAP it is not feasible to allow re-entry.
Failure of a clinical course will also constitute unacceptable performance and will result in dismissal from the NAP.
Students at risk of not passing a course have the responsibility of seeking assistance from the course instructor or advisor. Please contact your NAP faculty if your grade drops below a B+ at any time during the semester.
Academic Advising:
See NAP Student Handbook Policy and Procedure Manual
Attendance Policies for class and clinical:
See NAP Student Handbook Policy and Procedure Manual
Post Baccalaureate Certificate in Forensic Nursing
For information, contact Dr, Catherine Zurawski catherine.zurawski@cedarcrest.edu
610-606-4606
Mission of the Graduate Nursing Program
The mission of the Cedar Crest College graduate nursing program is to educate and prepare nurse leaders who will advance evidence-based practice, education, and healthcare delivery to improve health outcomes for individuals, families, and communities within a global context.
Post Baccalaureate Certificate in Forensic Nursing
Forensic nursing can be defined as specialized care for patients experiencing acute and long-term health consequences associated with victimization or violence. Nurses educated in the principles of forensic science help victims of trauma, aid in the investigation of child abuse, elder abuse, human trafficking, and domestic violence. In addition, forensic nurses often play a role in death investigations for coroners and medical examiners. This certificate prepares RNs who work in settings where there is no formal forensic nursing position to apply this enhanced skill set to a multitude of areas-including inpatient, outpatient, community/ home health, schools and elder care facilities, coroner’s offices, corrections, and in mass disasters/ trauma.
Admission Requirements
- Completed online application form
- Bachelor’s degree in nursing from an accredited program
- Active, unencumbered Registered Nurse licensure in Pennsylvania
- Official transcripts from all previously attended institutions of higher education
- Completion of an interview with the Director of the program and/or representatives from the Graduate Nursing Program Committee.
Certificate in Forensic Nursing Expected Learning Outcomes (SLOs)
1.Provide competent, comprehensive, patient-centered, trauma-informed care using both independent and collaborative approaches to patients across the lifespan who have experienced abuse, sexual assault or have otherwise been victimized.
2.Incorporate fundamentals of forensic nursing practice to assess, plan, implement and evaluate care; educate and collaborate with patients to identify care goals; and coordinate and refer to outside agencies as appropriate.
3. Skillfully collect, preserve, and document physical and evidentiary findings using principles of forensic nursing to facilitate legal proceedings.
4.Provide objective, accurate, evidence-based testimony appropriate for medical documentation and judicial proceedings.
5.Incorporate evidence-based interventions to address public health issues within forensic contexts, such as violence prevention, victim advocacy, and community interventions.
6.Utilize epidemiological methods and data analysis techniques to identify health disparities and formulate evidence-based strategies for promoting the health and well-being of diverse populations affected by forensic issues
Program of Study
Courses required for the post-baccalaureate Certificate in Forensic Nursing:
MSN 557 Forensic Nursing 1 – 3 credits
SWK 507 Victimology – 3 credits
FSC 559 Legal Issues and Evidentiary Collection – 3 credits
MSN558 Forensic Nursing 2 – 4 credits (3 credits didactic, 1 credit clinical (56 hours)
*A mandatory 1-2 day On Campus Immersion is required that will evaluate competency with patient interaction and physical examination, evidence collection and preservation, documentation, and interdisciplinary collaboration.
School Nurse Certification Program
For information, contact Dr. Nancy Roberts, School Nurse Certification Program Advisor, at nroberts@cedarcrest.edu, 610-606-4606.
At Cedar Crest, students have the opportunity to practice leadership and problem-solving skills that are necessary to excel and advance in today’s professional fields. Cedar Crest College emphasizes an environment where individual growth and professional skills are integrated so that our students acquire the knowledge, attitudes and abilities that they need to succeed. The multi-disciplinary School Nurse Certification Program provides the necessary knowledge and practical skills to those who serve the health needs of school-age children.
An applicant to the school nurse certification program must hold an unencumbered active professional nursing license with one year of professional experience and a baccalaureate degree. An undergraduate GPA of 2.5 is required for admission. A GPA of 3.0 is required for progression in the program and Pennsylvania School Nurse Certification.
Courses Required for the School Nurse Certification Program
All courses are offered Online
EDU 559 Curriculum and Instruction for the English Language Learner 3 credits
OR
EDU 516 Teaching for Social Change 3 credits
OR
MSN 531 Curricula in Nursing Education 3 credits
SPE 541 The Exceptional Child: Special Education Process: PreK-Transition 3 credits
SPE 544 Adaptations, Modifications, and Assistive Technology 3 credits
SNC 500 Methodology in School Health Services 3 credits
SNC 505 School Nurse Practicum 5 credits /105 clinical hours
All candidates for the school nurse certificate, both in state and out of state, must take SNC 500 and 505 in sequential order and within one academic year. Pennsylvania Department of Education (PDE) requires the following for certification in PA:
Six credits of college course work in mathematics; three credits in English composition; and three credits in American or British literature. It is a requirement of Cedar Crest College that the student earn a grade of C or higher in these courses.
For more information, contact the School of Adult and Graduate Education (SAGE) at sage@cedarcrest.edu.
Clinical Requirements
All students must provide proof of RN licensure from the state in which they will complete their practicum and to which they are applying for certification:
- Report of Health Evaluation and Medical History
- Immunizations, Titers, Current PPD and Influenza Vaccine
- Drug and Alcohol Screen
- CPR certification must be Basic Life Support CPR with AED for Healthcare Providers through the American Red Cross or the American Heart Association
- Proof of Health Insurance
- FBI Criminal History Clearance
- Child Abuse History Clearance
- PA Criminal History Clearance
Prospective and current nursing students must submit criminal background checks that meet the requirements of the nursing program before beginning nursing courses and annually thereafter.
Prospective nursing students with criminal records must disclose their records and schedule a meeting with the Dean of the School of Nursing upon admission to Cedar Crest College.
Any student not clinically cleared for clinical courses by the last day of the add/drop period will be automatically dropped from the course. Late clearances cannot be accepted.
Expenses (in addition to comprehensive and special fees)
Students are responsible for all fees involved when obtaining the clinical requirements, secured electronic file management, books, professional and scholarly activities, and certification fees.
Departmental Review for Field Placement
Students majoring in Education, Nuclear Medicine, Nursing, Nutrition or Social Work are required to complete a field practicum or clinical experience. Because this requirement necessitates working with the public in a professional setting, it is important that the student has advanced interpersonal skills, mature judgment, and appropriate professional demeanor. Thus, faculty in these programs will review students prior to the practicum and make appropriate recommendations up to and including removal from placement.